ThaiHealth and Key Health Agencies in Thailand Hosted the “Thai UHC Journey Workshop 2024” to Share Health Promotion Movements and Challenges in the 21st Century, Highlighting the Use of Sin Taxes to Promote Health in Thailand
The Thai Health Promotion Foundation (ThaiHealth) together with the Ministry of Public Health (MOPH), the National Health Security Office (NHSO), the National Health Commission Office (NHCO), the Enhancing Leadership in Global Health Thailand Programme (WHO-CCS EnLIGHT), the International Health Policy Program Foundation (IHPF), and the ThaiHealth Academy jointly organized the “Thai UHC Journey Workshop 2024” under the theme “Health Promotion: A Transformative Path towards Sustainable Health and Well-being from November 4-8, 2024, at the ThaiHealth Center in Bangkok, Thailand.

Dr. Prakasit Kayasith, Senior Assistant CEO and Director of Partnership and International Relations, ThaiHealth, mentioned that “Now in its fourth iteration, the Thai UHC Journey Workshop 2024 aims to share lessons and experiences of Thailand’s overall health system and Universal Health Coverage (UHC) with low-and middle-income countries while encouraging discussions and networking to promote health and well-being.
We believe that Thailand’s experiences, best practices, and lessons in health promotion can serve as valuable knowledge for other countries. Additionally, this five-day workshop is expected to deepen understanding of health promotion, strengthen health systems, and UHC, contributing to improving health and well-being worldwide and lay the foundation for international collaboration in the years ahead.”
Speaking on the theme “Health Promotion: A Transformative Path Towards Improved and More Sustainable Well-being”, Dr. Prakasit stated:
“Health” was defined by WHO in 1946 as ‘a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.’ Later in 1986, the Ottawa Charter described “health promotion”as ‘the process of enabling people to increase control over and to improve their health.’ In 2005, Bangkok Charter for Health Promotion in a Globalized World expanded on this as ‘the process of enabling people to
increase control over their health and its determinants, thereby improving their health.’ Therefore, health promotion is not limited to disease prevention but rather involves creating environments and encouraging individuals to care for their physical, mental, and social well-being. It is not a responsibility exclusive to the public health sector but involves all sectors.
Health promotion – a crucial concept in public health – can be achieved through two primary approaches. Specifically, the individual/service-based approach centers on health services provided by healthcareprofessionals, such as physicians and nurses, focusing on the disease prevention and health education of individuals on self-care and encourage behavioral changes. The population/result-based approach emphasizes broad-based multi-sectoral actions, focusing on community or population health. It highlights the social responsibility to create environments conducive to health and to address social and environmental determinants affecting health. It is founded on the international recognized Ottawa Charter’s five strategic actions.
In practice, the successful implementation of health promotion draws on both approaches to achieve comprehensive and sustainable outcomes. This lies the inherent complexity of health promotion, so it necessitates multi-sectoral collaboration – the government, academia, private sector, and civil society – to foster a healthy society.
The Ottawa Charter for Health Promotion, an internationally adopted framework for health promotion, underscores that health promotion is not necessarily limited to disease treatment but rather is a multi-faceted process aimed at enhancing health and quality of life. It identifies five strategies or priority action areas for health promotion as follows: 1) building healthy public policy, such as tobacco control laws and harmful products taxation ; 2) creating supportive environments, such as parks and safe communities; 3) strengthening community actions, such as empowerment of community engagement in planning and addressing health-related issues; 4) developing personal skills, such as provision of education about nutrition and stress management; and 5) reorienting health services towards disease prevention and health promotion over curative services.

Establishment of ThaiHealth
The Thai Health Promotion Foundation (ThaiHealth) was established under the Thai Health Promotion Foundation Act B.E.2544 (2001). It is mainly tasked with advancing health promotion initiatives in Thailand and engages with various agencies and partners across all sectors through its Tri-Power Strategy. ThaiHealth refers
“health promotion” to any action aimed at fostering physical, mental, and social well-being among individuals by supporting individual behaviors, social conditions, and environments which contribute to physical well-being, mental wellness, social and spiritual well-being, and improved quality of life.
ThaiHealth’s Health Promotion Working Model
ThaiHealth adopts a modern approach to health promotion grounded in Green and Tones’ model of health promotion (2012) and the Ottawa Charter for Health Promotion’s five priority action areas. This approach encompasses five main strategies as follows: 1) building healthy public policy; 2) creating supportive environments; 3) strengthening community actions; 4) developing personal knowledge and skills; 5) reorienting healthcare services towards prevention and health promotion. To achieve holistic public health across four dimensions, ThaiHealth’s working model is structured around the following five areas.
1. Building Healthy Public Policy: This serves as one of the core strategies for enhancing population health. Specifically, it involves advocating for health to be a critical agenda for policymakers across various sectors at all levels – local to national. This aims to foster their awareness of the health impacts of policies and ensure accountability for the outcomes. It involves developing diverse and coordinated health promotion policies, such as legislation, implementation of taxation measures, organizational restructuring, or launching campaigns, to achieve far-reaching impacts. Examples are Sugar-Sweetened Beverage Tax (SSB tax), alcohol control laws, and physical activity promotion campaigns.
2. Creating Supportive Environments: Health promotion contributes to cultivating living and working environments which are safe, appealing, fulfilling, and joyful. Assessing health impacts of rapid changes – technological advancements, work practices, energy production, and urbanization – is imperative. Proactive actions must be taken to yield the maximum benefits for the public health. The preservation of natural and built environments, together with the conservation of natural resources, is integral to health promotion strategies. Simply put, a supportive environment encompasses safety, livability, and the promotion of physical and mental well-being.
3. Strengthening Community Actions: This involves concrete and effective actions at the community level, such as determining priorities, decision-making, planning, and implementation, to achieve health objectives.The core of this process lies in empowering communities to independently make decisions and implementhealth-related activities. Community development necessitates utilizing local resources – both human and material – to strengthen the community and foster its involvement in health care.
4. Developing Personal Skills: This aspect promotes self-improvement and social development through information sharing, health education, and the cultivation of life skills. Additionally, it fosters lifelong learning to equip individuals to accommodate or navigate through changes and maintain their health over time. It also underlines the importance of sports and physical activities, incorporates digital technologies for accessing health information and services, and reinforces the significance of basic health care.
5. Reorienting Health Services towards P&P: This area shifts the focus of health services from predominantly
curative care to prevention and health promotion. Simply put, health agencies should prioritize health
promotion and disease prevention over curative care in line with the concept of holistic health care. This approach takes into account health determinants, recognizing that health is shaped by not only health factors but also social, economic, and cultural factors. Health agencies should also be engaged in health promotion efforts, such as providing health check-ups, administering vaccines, and offering health counseling.
Key Threats and Trends in 21st-Century Global Public Health
Many major factors shape the current and future global health system. 1. The surge in health expenditures.
Worldwide, healthcare expenses are continually rising, potentially stemming from advancements in medical innovations, new technologies, and the growing prevalence of chronic diseases. 2. Widening global health
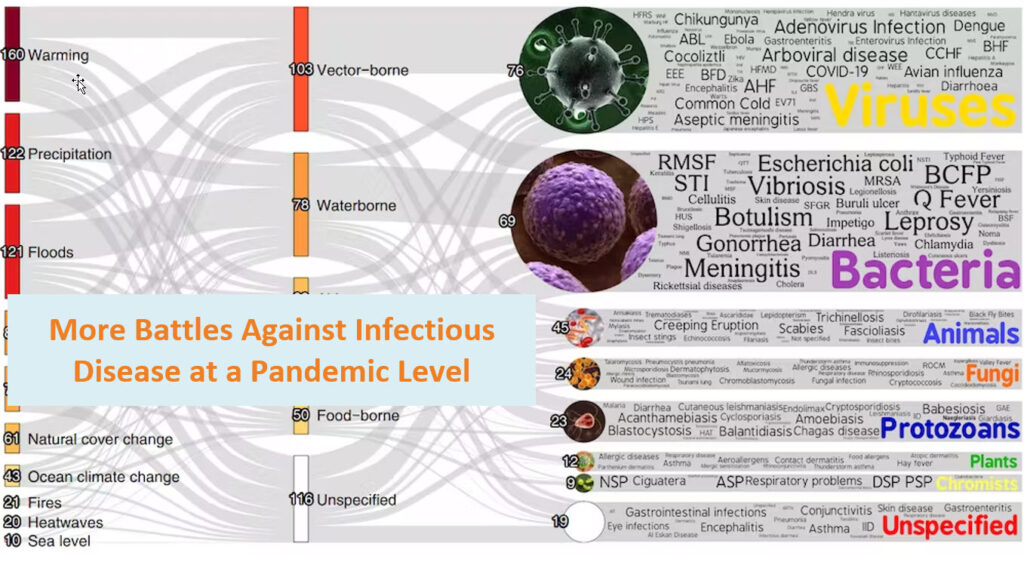
disparities still remain a global issue, with the economically disadvantaged often having limited access to healthcare services and suffering from poor health. 3. A shortage of healthcare personnel compromises the quality of healthcare services. 4. Mental health crisis is escalating worldwide and linked to various factors, such as workplace stress, economic pressure, social changes, and pandemics. 5. Digital innovations brought unprecedented benefits and at the same time posed challenges, such as unequal access and concerns over health data security. 6. Economic-related issues, such as inflation, climate change, and energy crises, directly impact the health system. 7. Alternative care models, such as alternative medicine or self-care, are a growing trend. ASEAN also faced many threats include escalating climate change/global warming, battles against infectious diseases at a pandemic level, mental health crises, demographic shifts, and non-communicable diseases (NCDs), such as tobacco and alcohol use, overweight and mental illnesses, and air pollution.
These challenges and trends impact various dimensions of the health system as follows:
1) access to healthcare services, with some groups facing greater difficulty in accessing those services; 2) quality of healthcare services, which may be compromised due to a lack of personnel and resources; 3) rising health expenditures; and 4) sustainability of the health system, which is at risk in the long term.
Addressing these threats and trends necessitates actions across different levels. At the policy level, it is imperative to establish healthy and prevention policies, invest in the health system, and foster equitable access to healthcare services. At the community level, community involvement in healthcare should be promoted while collaborative networks should be fostered across different sectors. At the individual level, health literacy and healthy behaviors should be promoted.
What actions can we take to contribute to health promotion?
1. Mobilizing domestic resources: Revenue derived from taxes or fundraising initiatives can be drawn on for health promotion and national development. A focus should be on collaborative efforts, such as the International Network of Health Promotion Foundations (INHPF), to maximize resource utilization. 2. Easing public health burdens and promoting sustainable development: Reducing health-related issues or damages which strain the public health, economy, and society can increase the sustainability of the public health system and alleviate long-term challenges. 3. Preventing and preparing for potential diseases and health risks: Prevention and preparedness can minimize the impact of emerging diseases and risks on health of individuals. This approach focuses on addressing social and business-driven risk factors, such as air pollution or marketing practices which cultivate unhealthy behaviors.

Mr. Rungsun Munkong, International Relations Expert, discussed Thailand’s health promotion, covering ThaiHealth’s structure and operations, its funding derived from sin taxes to advance the country’s health promotion, and the adoption of the Ottawa Charter. Specifically, he noted that Thailand has a population of 69,626,000. The leading causes of mortality among Thais are NCDs — such as heart disease, diabetes, cancer, and chronic respiratory diseases — accounting for 77% of total deaths in the country, approximately 400,000 fatalities per year. Given the alarming figure, the country bears a significant economic burden, with annual healthcare costs for NCDs reaching $6 billion USD, equivalent to 2.2% of its GDP.
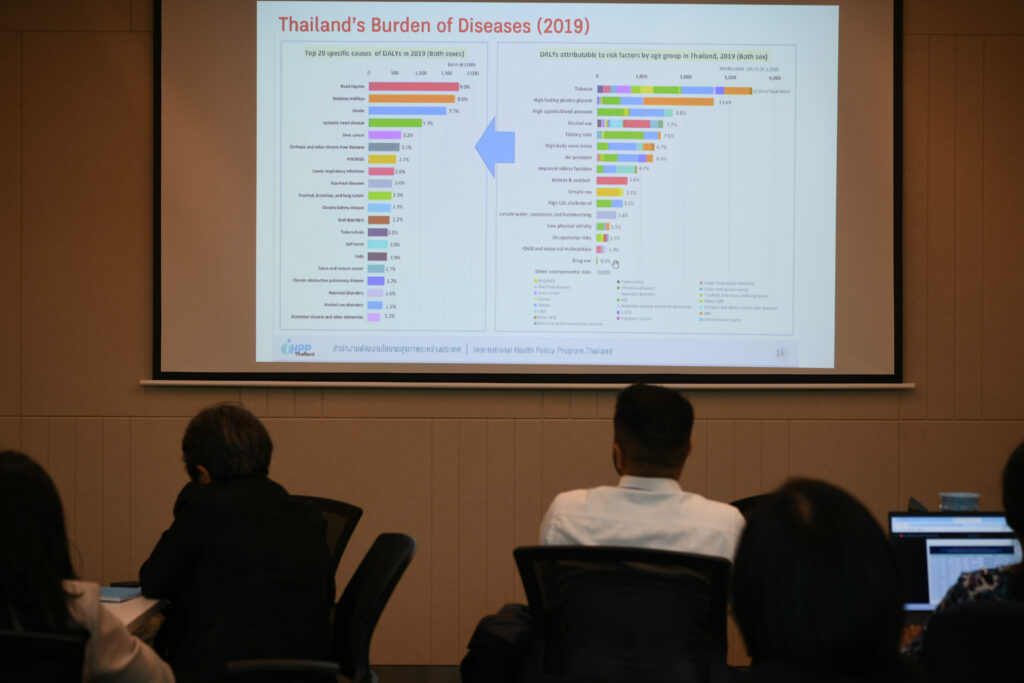
In addition, other major cause of death includes accidents, especially road accidents, and infectious diseases such as tuberculosis and respiratory infections, which contribute to mortality and disability. Contributing risk factors to NCDs and other health issues encompass risky behaviors — such as smoking, alcohol consumption, unhealthy diets, and physical inactivity — as well as unhealthy environments, such as air pollution and inadequate access to clean water, and social determinants, such as poverty and limited access to healthcare services. Thailand’s approach to health promotion and prevention of NCDs involves a multi-sectoral strategy, aiming toreduce the prevalence of NCDs and improve quality of life. Effective implementation hinges on collective efforts across all sectors, which will contribute to sustainable outcomes.

The Thai Health Promotion Foundation (ThaiHealth) was established under the Health Promotion Foundation Act B.E. 2544 (2001) as a semi-autonomous governmental agency. ThaiHealth is tasked with encouraging, supporting, and funding various sectors to advance health promotion. The goals are to reduce morbidity and premature mortality, foster behavioral and belief changes, and create environments conducive to a higher quality of life.
ThaiHealth’s funding is derived from a 2% surcharge on excise taxes on tobacco and alcohol. This dedicated taxation model serves as an innovative health financing mechanism. Each year, ThaiHealth allocates its budget to support over 3,000 health promotion projects.
ThaiHealth’s Board of Governance is composed of multi-sectoral members and chaired by the Prime Minister. Its members include representatives from government ministries and independent experts in various areas. The Board is responsible for formulating strategic direction as well as approve organization’s policies and budget.
ThaiHealth’s Vision is: “All people living in Thailand have capability and live in society and environment conducive to good health”. Its Mission is “to inspire, motivate, coordinate, and
empower individuals and organizations in all sectors for the enhancement of health promotive capability as well as healthy society and environment to support health promotion movement in Thailand.”
ThaiHealth’s 10-year goals aim to improve the comprehensive well-being for Thai people across four dimensions. Specifically, its goals are encapsulated in 7+1 strategic priority areas, encompassing tobacco, alcohol and substance abuse, healthy diet, physical activity, road safety, mental health, environmental pollution, and emerging health issues. The focus of these efforts is on addressing health disparities, enabling access to health knowledge and care, and ultimately enhancing the overall health of Thai people. These goals are pursued through 15 priority areas. ThaiHealth adopts a multi-sectoral approach, working in tandem with a wide array of stakeholders such as government agencies, private companies, NGOs, educational institutions, and communities.

Its strategy is grounded in an integrative approach known as “Tri-power Strategy”, comprising “Knowledge Power, Social Power, and Policy Power.” This is rooted in the belief that collective efforts and shared goals among all sectors can contribute to a healthy and well-being society. Each year, ThaiHealth supports upwards of 3,000 projects and has collaborated with over 20,000 partners cumulatively.
This integrated approach draws on creativity and collective action to drive social change and achieve sustainable impacts.

Tobacco control policies, advocated by ThaiHealth and its partners to address tobacco-related issues, align with the WHO Framework Convention on Tobacco Control (WHO FCTC). To address tobacco-related issues in Thailand, ThaiHealth has implemented strategies aimed at reduce the number of new smokers, alleviating the health impacts, and fostering a smoke-free society. In particular, four strategies have been adopted.
1. Advocating for tobacco control laws and regulations: ThaiHealth works closely with relevant agencies, such as the National Tobacco Control Committee and the Ministry of Public Health, to advocate for and effectively enforce tobacco control laws.
2. Tobacco control planning: long-term plans are established with specific goals, and budgets are allocated to facilitate the implementation.
3. Knowledge generation: ThaiHealth supports research and develops knowledge about tobacco-related issues while working to raise public awareness about the dangers of smoking through knowledge dissemination.
4. Promoting public engagement: ThaiHealth collaborates with civil society organizations, media, and other sectors to campaign for smoking cessation and foster a smoke-free society in Thailand.
In addition, ThaiHealth works in tandem with various healthcare professionals in tackling tobacco use. In particular, the Thai Health Professional Alliance against Tobacco acts as the central body, uniting efforts among healthcare professionals in various disciplines — such as physicians, dentists, pharmacists, nurses, and physicaltherapists — to address smoking-related health issues. Their efforts include counseling services, smoking cessation campaigns, and policy advocacy.

Despite that, Thailand faces two challenges in tobacco control, which undermine its efforts to reduce smoking rates and foster a smoke-free society. 1. Shortage of dedicated personnel for provincial tobacco control: Each province lacks trained and dedicated personnel, thereby compromising the efficiency and continuity of tobacco control measures. 2. Tobacco industry interference: The tobacco industry undermines tobacco control policies and measures through various strategies, such as offering financial incentives or forging relationships with non-health organizations, thereby obstructing effective implementation. 3. Rising trend of youth smoking: A considerable number of young people aged 15-24 are smoking, particularly e-cigarettes, with the figure expected to rise annually. This poses a serious concern, for the youth are a primary target for the tobacco industry.
Road safety policies, advocated by ThaiHealth and its partners to mitigate road accidents and fatalities, are in line with the WHO’s global plan to halve road accidents by 2030. The following are key policies: 1. Enforcement of laws on speed limits and drunk driving, such as mandating appropriate speed limits and prohibiting drunk driving; 2. Advocating for 100% helmet use; 3. Mandatory seat belts in public transport, requiring all passengers to wear seat belts to minimize the risk of injuries in accidents; 4. Ban on the registration of new double-decker buses due to their high risks of accidents; and 5. Improving road infrastructure to ensureroad safety through various measures, such as installing traffic signs, pedestrian crossings, and improving traffic lights.

Meanwhile, the physical activity initiatives promoted by ThaiHealth and its partners primarily seek to increase physical activity among people of all ages to prevent chronic diseases and promote good health. These efforts are pursued through the following initiatives: 1. Promoting physical activity for all age groups, with regular exercise programs organized for individuals of all ages and genders; 2. Creating healthy spaces, such as parks, playgrounds, and walking/running tracks; 3. Organizing national events, such as marathons and National Exercise Day; 4. Fostering international collaboration, such as ThaiHealth’s collaboration with the WHO and international organizations to promote physical activity; and 5. Advocating for physical activity policies, such as global action plan and national action plan for physical activity.
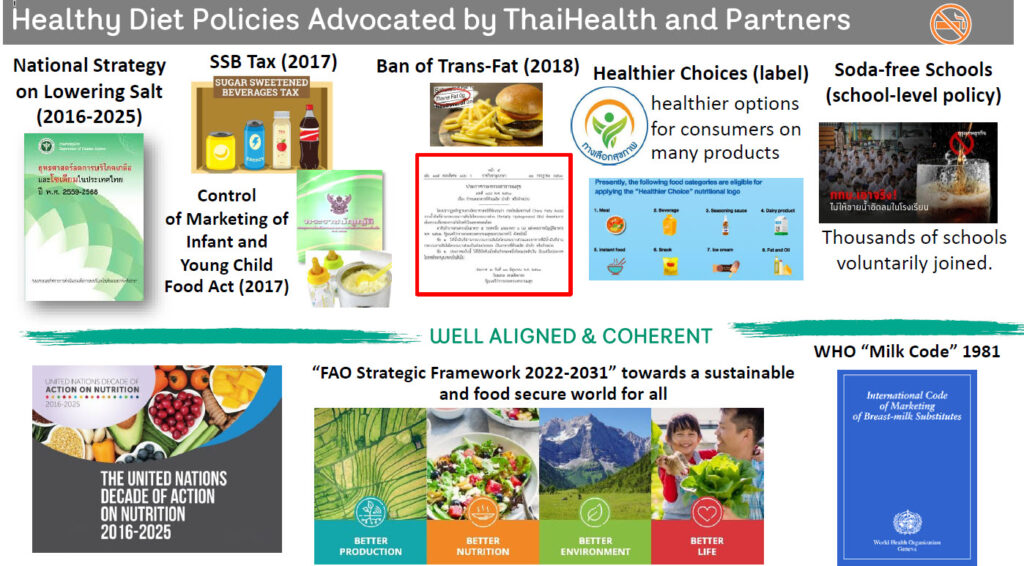
Additionally, ThaiHealth has joined efforts with its partners to advocate for healthy diet policies aimed at improving the health of Thai people. Notable examples include the following initiatives: 1. Sugar sweetened beverage tax (2017), which imposes a tax on sugar-sweetened beverages to encourage product reformulation and discourage consumption; 2. Ban on trans fats (2018), which prohibits the use of trans fats in all foods to mitigate the risk of cardiovascular diseases; 3. Nutrition labeling (“healthier choices” logo), which mandates
clear nutrition labels to enable consumers to make healthier choices; 4. Soda-free schools, aiming to encourage schools to ban the sale of sugar-sweetened beverages to ensure healthier habits among students; 5. Regulating food marketing to children, monitoring the advertising and promotion of unhealthy food to children; and 6. Promoting local fruit and vegetable, encouraging the consumption of fresh, seasonal, healthy local fruit and vegetable.
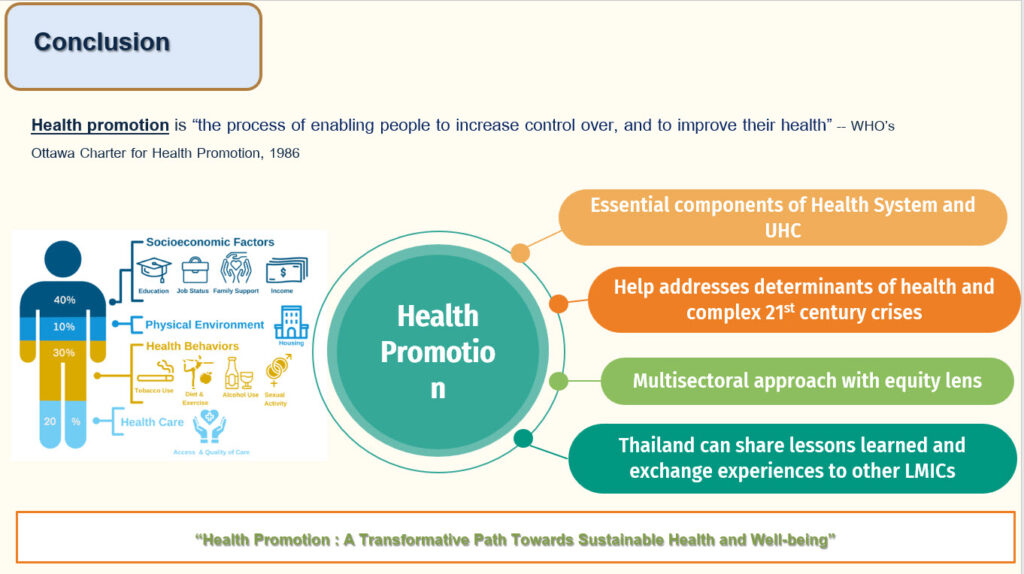
Conclusion
ThaiHealth’s strategies focus on addressing risk factors of NCDs, such as smoking, alcohol consumption, high-fat diets, and inadequate physical activity. ThaiHealth has utilized multi-sectoral approach, collaborating with all sectors to tackle health issues. Specifically, the efforts involve fostering community actions and social movements for health, supporting research to gather scientific data and evidence and advocating for the adoption and implementation of healthy policies. It aims to create environments conducive to good health as well as promoting healthy behaviors.
////////////